Breast Cancer Surgery & Partial Breast Reconstruction
At the core of Mr Ibrahim’s practice is a commitment to providing holistic, patient-centred care for those facing breast cancer. As a specialist Oncoplastic Breast Surgeon, he offers advanced techniques that prioritise both complete cancer removal and the best possible aesthetic outcome. For patients requiring breast-conserving surgery (a lumpectomy or wide local excision), he specialises in sophisticated oncoplastic techniques to reshape the breast immediately, avoiding deformity and often improving its overall shape.
1. Wide Local Excision (WLE) with Oncoplastic Reconstruction
What is it?
A Wide Local Excision (WLE) removes the cancerous lump along with a margin of healthy tissue. An oncoplastic reconstruction is performed in the same operation to fill the resulting defect and reshape the breast, preventing a visible dent or distortion. This approach is often called a Therapeutic Mammoplasty.
The Surgical Journey:
- Planning: Mr Ibrahim meticulously plans the surgery with you, marking the skin to design how the breast will be reshaped after the cancer is removed. The incisions often follow the patterns of a breast reduction or uplift.
- The Procedure: Under general anaesthetic, the cancer is first removed with clear margins (confirmed during surgery). Then, using the principles of cosmetic breast surgery, the remaining breast tissue is rearranged and the skin is tightened to create a smaller, lifted, and symmetrical breast. The nipple may be repositioned if needed. The same procedure can often be performed on the opposite breast to achieve perfect symmetry.
- Best For: Patients with moderate to large breasts where removing the cancer would leave a significant defect. It turns cancer surgery into an opportunity for a breast uplift and improved symmetry.
Benefits:
- Superior Cosmetic Result: Avoids a crater deformity; often leaves the breast perkier and more youthful.
- Improved Symmetry: Matching the opposite breast is part of the single operation.
- Oncologically Safe: Allows for larger excisions with clear margins while maintaining breast form.
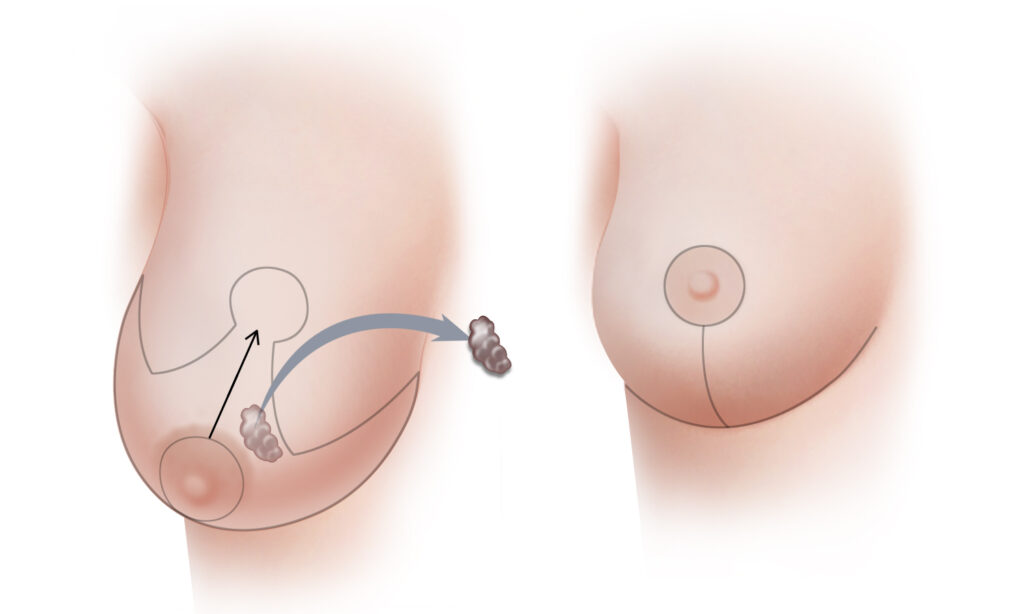
2. Partial Breast Reconstruction with a Chest Wall Perforator Flap
What is it?
For patients with smaller breasts where a therapeutic mammoplasty is not suitable, or when the cancer is located in an area difficult to reshape with standard techniques, Mr Ibrahim can reconstruct the partial defect using your own living tissue. A Chest Wall Perforator Flap involves moving a small island of skin, fat, and blood vessels from the chest wall adjacent to the breast (e.g., from the side/axilla or underneath the breasts) to precisely fill the surgical cavity.
The Surgical Journey:
- Planning: Advanced imaging may be used to map the tiny blood vessels (perforators) around the breast. Mr Ibrahim designs a small, well-hidden flap based on one of these vessels.
- The Procedure: After the cancer is removed, the pre-marked flap of tissue is carefully elevated, keeping its tiny blood supply intact. This living tissue is then rotated into the defect, like filling a hole with an identical, matching puzzle piece. The donor site is closed directly.
- Best For: Patients with small to medium-sized breasts, defects in the lower or outer breast, or those who desire autologous (own tissue) reconstruction without a distant donor site.
Benefits:
- Perfect Match: The reconstructed area uses local fat and skin, which ages naturally with the breast.
- Minimal Donor Site Morbidity: The tissue is taken from an adjacent area, leaving a single, well-hidden scar.
- No Muscle Damage: As a true perforator flap, the underlying chest muscle is preserved, leading to a faster, less painful recovery.
Your Oncoplastic Consultation:
Mr Ibrahim works within a Multidisciplinary Team (MDT). Your case will be discussed with oncologists and radiologists to plan the best treatment sequence. In your consultation, he will explain your specific cancer surgery and the reconstructive options available to you, ensuring you feel informed, supported, and confident in your personalised care plan.
Mastectomy with Reconstruction: Either using implants or your own tissue (autologous flap from the abdomen, thigh, or back) to rebuild a natural-looking breast. Mr Ibrahim is one of the few plastic surgeons with advanced fellowship training in complex microsurgical free flap reconstruction (e.g., DIEP flap).
- Symmetry Surgery: Procedures on the opposite breast to match the reconstructed side.
What to expect?
A consultation with Mr Ibrahim will involve a detailed discussion of your diagnosis (if applicable), goals, and all suitable options. He will explain the specific procedure, the recovery pathway (which varies greatly between implant and flap reconstruction), and the long-term outlook. As an NHS consultant, he provides the same gold-standard, multi-disciplinary approach to care in the private setting.
FAQ
1. What is partial breast reconstruction, and when is it performed?
Partial breast reconstruction is a specialised procedure to restore the shape, volume, and contour of the breast after a Wide Local Excision (WLE) or lumpectomy for breast cancer. It is typically performed at the same time as your cancer surgery (immediate reconstruction) and is mostly is followed by radiotherapy.
2. What are the main benefits of having reconstruction at the same time as my WLE?
Immediate partial reconstruction aims to preserve the natural appearance of your breast from the outset. This can lead to superior aesthetic outcomes, minimise the psychological impact of losing breast tissue, and often means one less major surgery in the future. It is about restoring wholeness as part of your cancer treatment journey.
3. What techniques are used for partial breast reconstruction?
The technique is personalised to your defect, breast size, and goals. Common methods include therapeutic mammaplasty (breast reduction or lifting techniques to rearrange your own tissue), local glandular flaps (moving nearby breast tissue to fill the defect), and delayed fat grafting (lipomodelling) in a separate session.
4. I need radiotherapy. Can I still have immediate reconstruction?
Yes, in many cases. However, radiotherapy can cause tissues to change in texture and shrink over time. Mr. Ibrahim will discuss this with you in detail. Techniques are often chosen with this in mind—such as using your own resilient breast tissue—and occasionally you may need a minor revision procedure after radiotherapy is complete to fine-tune the final shape.
5. What is fat grafting (lipomodelling), and how does it help?
Fat grafting is a delicate technique where fat is gently liposuctioned from another area of your body (like the abdomen or thighs), purified, and carefully injected into the breast to correct contour irregularities, improve skin quality, and add volume. It is often used as a secondary “refinement” procedure to achieve a soft, natural result.
6. What is the recovery like compared to a full mastectomy?
Recovery is generally shorter and less intensive than after a full mastectomy with reconstruction. You can expect to go home after 1-2 days. There will be some discomfort, bruising, and swelling, but most women return to light activities within 1-2 weeks. You will need to wear a supportive bra and avoid strenuous exercise for 4-6 weeks.
7. Will I need surgery on my other breast for symmetry?
You do not need any symmetrising procedures with chest wall perforator flap for partial breast reconstruction.
on the other hand for breast reduction or lift techniques, to achieve a balanced and symmetrical appearance, a procedure on the opposite breast—such as a breast reduction, or lift (mastopexy)—is often recommended and can usually be performed during the same operation. This is discussed thoroughly during your consultation to align with your desired outcome.
8. Why is it important to choose a surgeon with oncoplastic expertise?
Oncoplastic surgery combines the precise cancer removal of oncology with the advanced reconstructive artistry of plastic surgery. As a Consultant Oncoplastic and Reconstructive Breast Surgeon, Mr. Ahmed Ibrahim is uniquely dual trained in both disciplines. This ensures your cancer treatment is never compromised while achieving the best possible aesthetic and psychological result.



