Breast Reconstruction with Back Muscle (Latissmus Dorsi Flap)
Breast Reconstruction with a Latissimus Dorsi (Back Muscle) Flap
A Natural Autologous Reconstruction Option
A Latissimus Dorsi (LD) flap reconstruction is a well-established surgical technique to rebuild the breast after mastectomy for cancer or risk reduction. Performed by Consultant Plastic and Oncoplastic Breast Surgeon Mr Ahmed Ibrahim, this procedure uses your own living tissue—skin, fat, and muscle from your upper back—to create a natural-feeling and lasting breast mound.
What is a Latissimus Dorsi Flap Reconstruction?
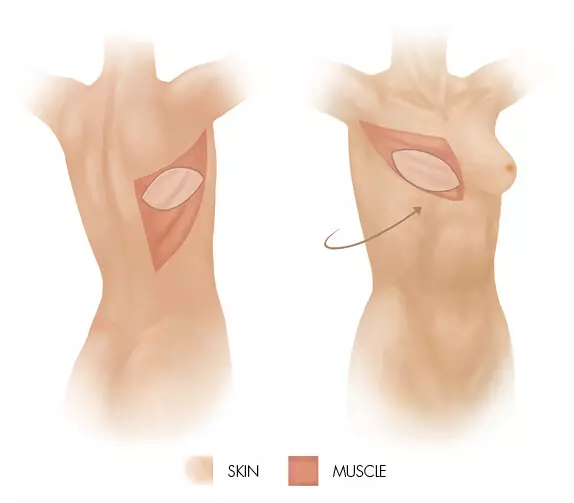
This is a type of autologous (using your own tissue) reconstruction. The latissimus dorsi muscle, along with an ellipse of overlying skin and fat from your back, is carefully mobilised while preserving its crucial blood supply. This tissue “flap” is then tunnelled under the skin to the chest to form a new breast. It is sometimes combined with a breast implant to provide adequate volume, when the back tissue alone is not thick enough.
The Ideal Candidate
You may be a suitable candidate for this procedure if:
You desire an autologous reconstruction but do not have sufficient abdominal tissue for a DIEP flap, or prefer to avoid abdominal surgery.
You have had prior radiotherapy to the chest wall or are likely to need it, as the well-vascularised back muscle brings healthy tissue to the area.
You need additional healthy skin and muscle to cover an implant securely, especially if your mastectomy skin is thin or damaged.
You are a non-smoker or can stop well in advance, as smoking severely compromises blood flow and healing.
Your Surgical Journey with Mr Ibrahim
Consultation: Mr Ibrahim will discuss your reconstruction goals, medical history, and oncological treatment plan. He will examine your back tissue and chest, explaining how the LD flap works, the role of the implant, and the scars on both the breast and back.
Procedure: The surgery is performed under general anaesthesia and can take 3-5 hours. Mr Ibrahim performs the mastectomy, after which harvests the flap and sculpts the new breast. It is often performed as an immediate reconstruction at the same time as mastectomy, but can also be delayed.
Hospital Recovery: You will typically stay in hospital for 3-5 days. One or two surgical drains are placed in the breast and back to prevent fluid collection. You will receive immediate support from the specialist breast care nursing team.
Home Recovery & Long-Term Results: Initial recovery involves managing discomfort and avoiding strenuous arm movements for 6-8 weeks. Scars on the breast and back will fade over 12-18 months. A second minor procedure (e.g., nipple reconstruction and symmetrisation of the opposite breast) is often performed later to refine the result. The reconstructed breast will feel natural and warm, but sensation will be different.
Realistic Expectations & Key Considerations
The LD flap offers a reliable, durable reconstruction with a natural drape. Key points to understand are:
Implant Requirement: An implant may be needed, carrying its own long-term considerations (e.g., potential for capsular contracture or future replacement).
Back Function: Most patients retain excellent back and arm function for daily life and sports, though some may notice a slight reduction in peak athletic power.
Scars: You will have a scar on your reconstructed breast and a horizontal scar on your back, usually placed within the bra line.
Symmetry: Perfect symmetry with the natural breast is challenging; a procedure on the opposite breast (reduction, lift, or augmentation) is often recommended to achieve the best match.
FAQ
1. How is an LD flap different from a "DIEP" or abdominal flap?
Both use your own tissue, but the donor site is different. The DIEP flap uses abdominal skin and fat without sacrificing muscle, leaving a tummy-tuck like scar. The LD flap uses back skin, fat, and muscle, and may require an implant. The choice depends on your body shape, lifestyle, and medical history.
2. In some cases, why is an implant needed with an LD flap?
If the latissimus dorsi muscle and the overlying back fat pad are not thick enough on their own to create an average-sized breast mound. The implant provides the necessary volume to match the opposite side.
3. What will my back be like after the muscle is moved?
The latissimus dorsi is a large muscle, but other muscles (like those in your shoulder) compensate well. Most people return to all normal activities, including swimming, gym, and golf. Some may notice reduced strength in activities like climbing or tennis, but this is often minimal. You will have a scar, and some may experience a slight contour change on the back.
4. What are the specific risks of this procedure?
In addition to general surgical risks, specific ones include:
Flap failure (loss of the tissue due to blood supply problems) – this is rare.
Back seroma (persistent fluid collection under the back scar) – very common, often requiring multiple drainages.
Shoulder stiffness or weakness.
If implant is used: Implant-related complications (capsular contracture, rupture, rotation) over the long term.
5. How does radiotherapy affect this type of reconstruction?
The LD flap is often chosen in cases requiring radiotherapy. The healthy, non-irradiated muscle brought from the back to recunstruct a breast on its own or covers the implant, which can reduce the risk of severe capsular contracture and implant-related problems compared to placing an implant directly under radiated skin.
6. What is the recovery timeline?
Hospital stay: 3-5 days.
Drains: Removed after 1-3 weeks, once output is low.
Driving: Avoid for 4-6 weeks.
Desk work: Possible in 4-6 weeks.
Light exercise: After 6-8 weeks.
Heavy lifting/gym: Avoid for 3 months.
7. Can I have a nipple-sparing mastectomy with an LD flap reconstruction?
This is sometimes possible if your cancer location and breast shape are suitable. It allows preservation of your natural nipple on the newly reconstructed breast mound. Mr Ibrahim will assess your eligibility.
8. Is this procedure available on the NHS?
Oncoplastic surgery combines the precise cancer removal of oncology with the advanced reconstructive artistry of plastic surgery. As a Consultant Plastic and Oncoplastic Breast Surgeon, Mr. Ahmed Ibrahim is uniquely dual trained in both disciplines. This ensures your cancer treatment is never compromised while achieving the best possible aesthetic and psychological result.



