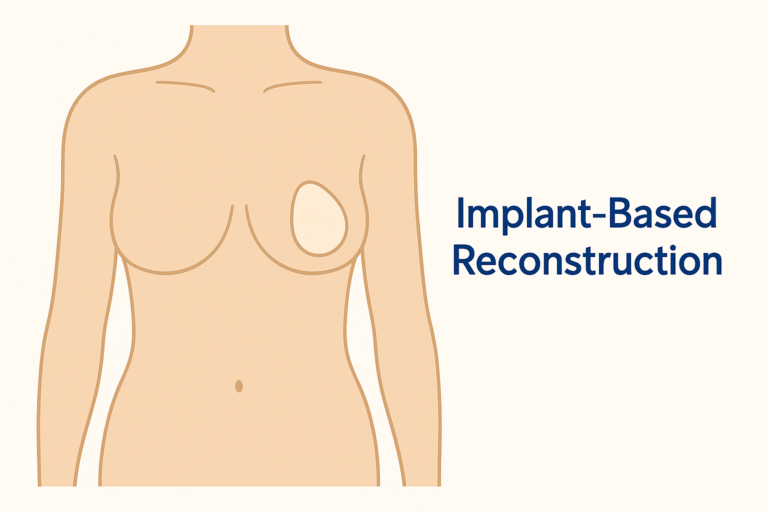
Implant-Based Breast Reconstruction
Recreating a Breast Mound with Implants
Implant-based reconstruction is a surgical technique that uses a silicone breast implant to recreate the shape and volume of the breast after a mastectomy. This approach can be performed in a single stage or, more commonly, in two stages using a tissue expander. It is known for its shorter initial operating time and recovery compared to procedures using your own tissue.
The Surgical Journey: One-Stage vs. Two-Stage
Your surgical plan will depend on the quality of your skin and tissue after mastectomy and your personal goals.
Direct-to-Implant (One-Stage) Reconstruction: In a single operation, Mr Ibrahim performs the mastectomy immediately places a permanent implant. This is suitable for patients with good skin quality who do not require radiotherapy.
Two-Stage (Expander-Implant) Reconstruction: This is the more common pathway, especially if the skin needs to be stretched or if post-mastectomy radiotherapy is planned.
Stage 1: After the mastectomy, a temporary tissue expander—a deflated, empty implant—is placed beneath the chest muscle. Over subsequent weeks in the clinic, this expander is gradually filled with saline via a small port to gently stretch the skin and muscle, creating a pocket.
Stage 2: Once the desired volume is achieved and the tissues have healed (often 3-6 months later, or after radiotherapy is complete), a second, smaller operation is performed. The expander is removed and replaced with a permanent silicone implant.
FAQ
1. Am I a good candidate for implant reconstruction?
This approach may be well-suited for you if you have sufficient healthy skin after mastectomy, desire a shorter initial surgery and recovery, have limited donor tissue for a flap, or prefer to avoid additional scars on other parts of your body. Mr Ibrahim will assess your specific anatomy and cancer treatment plan to advise if it is your safest and most appropriate option.
2. What types of implants are used?
Most commonly, silicone gel implants are used for their natural feel and appearance. Mr Ibrahim will discuss the options regarding shape (round or anatomical) and surface texture, helping you choose based on your body frame and desired outcome.
3. What is the recovery like?
Hospital Stay: Typically 1-2 nights.
Initial Recovery: You will have surgical drains and wear a supportive bra. Discomfort is managed with medication. If you have an expander, the filling process in clinic is usually well-tolerated.
Returning to Activities: Most patients return to light, desk-based work within 2-3 weeks. Strenuous activity and heavy lifting must be avoided for at least 6 weeks.
After Stage 2: The exchange surgery has a shorter recovery, often with a return to normal activities within 2 weeks.
4. What are the potential risks and long-term considerations?
All surgery carries risks of bleeding, infection, and anaesthesia complications. Specific risks include:
Capsular Contracture: The formation of tight scar tissue around the implant, which can cause firmness, discomfort, or visible distortion. This is the most common reason for revisional surgery.
Implant Rupture or Leakage: Modern implants are very durable, but they are not lifetime devices. Routine monitoring is advised.
Implant Malposition or Rippling: Where the implant shifts or its edges become visible.
Need for Future Surgery: Implants may need to be replaced or revised in the future.
5. Can I have implant reconstruction if I need radiotherapy?
Radiotherapy can increase the risk of complications like capsular contracture and poor wound healing with implants. In many cases, a two-stage approach is used, where the temporary expander is placed to preserve the skin space. The permanent implant is placed several months after radiotherapy is complete, once the tissues have recovered. Mr Ibrahim will carefully plan the timing.
6. How long do breast implants last? Do they need to be replaced?
Breast implants are durable medical devices, and can be lifetime devices if the changes are tolerated and accepted by the patients. While many implants last for 10-15 years or longer without issue, the likelihood of requiring replacement or revision surgery increases over time. Reasons for future surgery can include capsular contracture, implant rupture, rippling, malposition, or a personal desire to change size. You should plan for long-term monitoring of your implants.
7. Will I have any sensation in my reconstructed breast?
It is important to have realistic expectations about sensation. A mastectomy necessarily disrupts nerves, leading to a permanent loss of normal nipple sensation and a significant reduction in skin sensation on the breast. Sensation may partially and gradually return in some areas over time, but it is highly variable. The goal of reconstruction is primarily to restore breast form and contour.
8. What are "acellular dermal matrices" (ADM) or "meshes," and are they used?
Acellular Dermal Matrices (ADMs) are specially processed biological or synthetic tissues used as an internal support scaffold in some implant reconstructions. They can help provide better definition to the lower breast fold (inframammary crease) and improve implant positioning. Mr Ibrahim will discuss whether using an ADM is appropriate for your specific surgical plan, as their use depends on your anatomy and the type of reconstruction.



